The pituitary gland is a half-breed in many ways. It is not really a part of the brain, but rather hangs beneath it.
Half of the gland, the posterior lobe, comes down from the brain and controls the body's water levels and secretes the hormone ADH — anti-diuretic hormone.
The other half, the anterior lobe, comes from tissues originating from the roof of the embryonic mouth, and controls sex hormone levels, lactation, growth hormone, natural body steroids, and the thyroid gland.
The pituitary is responsible for almost all of the body's hormonal systems, taking all of its cues from the hypothalamus, the hidden and very deeply located Grand Wizard of the brain.
The hypothalamus also controls such activities as body temperature, sexual drive, appetite, blood glucose levels, and sleep/arousal behavior patterns.
As elsewhere in the brain, tumors of the pituitary gland behave according to their cell of origin.
Most of these tumors are truly benign, although on occasion they may prove to be malignant (pituitary carcinomas).

The list of cells of the pituitary determines the tumor types, as well as the clinical syndromes related to each.
Almost all have the good prognosis that calls for total removal. On the other hand, almost all can eventually become “malignant by position.”
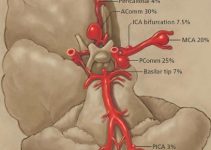
This is especially true when the tumors grow off to either side, involving the jam-packed structures behind both eyes, called the “cavernous sinuses.”
The pituitary gland is located exactly between these two structures, which contain the nerves that control eye movement and the major arteries that feed the brain (carotid arteries, the veins that drain the eyes and other nerve-related structures).
Therefore, these tumors may occasionally present the patient with double vision, or even something called “Pituitary Apoplexy” (severe sudden headache, loss of and/or double vision, or protruding eyeball).
Each tumor, because of its extraordinarily high hormonal output, creates a characteristic clinical syndrome that brings attention to the tumor.
Because the pituitary gland is located directly beneath the place where the nerves cross, coming from the eyes to the brain (the optic chiasm), many tumors also present — along with the hormonal problems listed below — loss of peripheral vision.
Table of Contents
Hormonal Problems
Gigantism: This syndrome is caused by pituitary tumors on the growth of hormone-secreting cells of the pituitary gland.
Lurch from the James Bond movie — large hands, protruding jaw, severe arthritis, huge size, protruding eyebrows, plus other systemic problems — is a classic example of gigantism.
Cushings Disease: This syndrome is caused by tumors on the ACTH (Adrenal Corticotrophin Hormone) secreting cells of the pituitary gland. Patients with this problem develop fat deposits in strange places (Moon face, Buffalo hump on the back of the neck), spontaneous scarring of the skin along the belly that looks striated, pimples in adults, high blood pressure and elevated body temperature.
These tumors are usually so small that the surgeon might have a difficult time finding the little “bad pearl” in the gland during surgery. This is the one time when small can be bad, especially if the surgeon is unable to locate and remove the tumor.
ACTH secreting tumors, although small and troublesome, are readily cured by surgery alone.
Prolactin Syndrome: This syndrome is caused by tumors on the prolactin-secreting cells of the pituitary gland.
The tumors are the most common of all the pituitary tumors. Production of breast milk in women who are not pregnant, loss of menstrual cycle, and loss of bone calcium are all hallmarks of this tumor.
When small, it may be cured; when large, it may cause visual problems and require other (e.g. radiation) therapy. Many women with this tumor visit their gynecologist thinking that they might be pregnant.
Growth hormone-secreting tumors may occasionally be treated with drugs, but most often must be removed surgically.
Non-Secreting Tumors: These tumors can be treated by surgery and/or radiation. These patients almost always have problems with vision, as the hormonally quiet tumor grows to oversized proportions, actually growing to the point of lifting up and stretching the optic nerves (especially where the nerves from both eyes cross as they travel to the brain).
The treatment of these tumors is variable. Prolactinomas are most often treated non-surgically with drugs that inhibit prolactin production (Parlodel).
Microprolactinomas never really grow over long periods of time and do not require surgery.
All pituitary tumors can be treated by radiation, especially with the improvements in focused beam radiation (linear accelerator and proton beam). The idea of radiosurgery originated in this venue.
One serious problem with radiation has been the loss of function in the remainder of the pituitary gland, requiring patients to depend on hormone supplements for the rest of their lives.
Another has been the inability to quickly reverse the visual loss in large tumors using radiation.
On the other hand, radiation has been used as a very successful adjunct in larger tumors that pose a threat to long term survival.
Surgery on Pituitary Tumors
The wonderful surgical achievement of the modern age is the combination of improved lighting, the surgical microscope, and computer-assisted navigational instrumentation now used in the O.R.
The pituitary gland lies just above the air spaces in the nose. In fact, the word “pituita” refers to the not so delicate production of “snot.” In medieval times in Europe, and in China today, it is thought that “pituita” was something good to get rid of, serving as a relief valve for bad humor of the brain.
In other words, spitting was good for the soul as well as one's health.
Thus, by traversing the structures just beneath the skull through the nasal cavities, brain surgery can be avoided and the risk of approaching the pituitary gland can be enormously reduced.
Decision Making for Pituitary Tumor Surgery
It's an emergency: patients who have a large pituitary tumor (and often don't even know about it) will occasionally develop a kind of pituitary “stroke,” called pituitary apoplexy.
This occurs after the tumor outgrows its blood supply and suddenly enlarges (due to swelling) after it infarcts (a type of local stroke), or begins bleeding within the tumor.
The enlargement causes severe headache and/or double vision because the nerves that control the eye located next to the gland are pressed upon.
It can also cause loss of vision (because the gland swells upward, pressing from beneath the optic nerves above). Surgical decompression is an emergency procedure because permanent blindness may result if left untreated.
Surgery Is the Best Way to Go
Cushing's Disease: Because the tumor is so small, a cure is possible when removed. Thus, surgery is the best way to go. Moreover, the remainder of the gland is left intact and will function normally thereafter.
Large tumors with liquified (necrotic) centers: In these cases, the surgery is easy, and the improvement is immediate. Any remaining tumor beyond the confines of the surgical field can be safely treated by other standard therapies (e.g. radiation therapy).
Medium-sized tumors: Still within the confines of the pituitary gland. As with Cushing's tumors, the tumor can be completely removed and the gland saved for normal function.
A ‘Hold' on the Surgery
Prolactinomas: Should always be treated initially with medication (anti-DOPA agents such as Parlodel, Bromocriptine, etc.).
Even large tumors that most need to be treated by either surgery or radiosurgery should be pretreated with these drugs to shrink the tumor away from vital brain structures before surgery should be contemplated.
Microprolactinomas: Surgically, nothing needs to be done for as long as possible. Some of these tumors appear to just sit there for years, even decades.
Extremely large tumors that cause little visual or other brain problems: In treating these tumors, particularly in older people, the physician should consider radiation therapy to stop their progression.
A surgical cure is usually not an option, due to the substantial surgical risk.