A TYPICAL SCENARIO:
The headaches she had been complaining about persisted for a few weeks, but no one worried.
Then, she awoke one morning with slurred speech and a wobbly gait. Now everyone was worried.
The family doctor was called; he recommended a CAT scan of the brain. After the scan, came the call: Go to the hospital right away! She has a subdural hematoma.
She had hit her head.
When?
No one in the family ever saw that, and she never said anything. She was sleeping last night safe and sound in her bed.
How could she have hit her head while she was asleep?
It didn't happen last night. It probably happened weeks ago. In fact, she probably didn't think much of it then.
It may even have been a minor bump, perhaps bumping her head on the car roof as she tried to get into the car during that rainstorm a few weeks ago.
Could that have caused all of this trouble?
This is the world of the subdural hematoma.
HOW DID IT HAPPEN?
One of the many interesting things about the brain is that the cells that we are born with are all that we ever get to work or play with.
Actually, a newborn has more brain cells than a fully mature adult!
The brain does not reproduce itself. And, as we age, the brain we were born with gradually shrinks.
On the other hand, the skull, once fully grown, never gets smaller.
The result is that our heads become very much like walnuts: the seeds dehydrate and shrink within the firm shell.
As the brain shrinks, it pulls away from its covering shell of bone (our skull); the intervening space is replaced by brain fluid (CSF).
At the same time, the blood vessels from the brain and that extend up into the skull become stretched, like rubber bands.
When they reach a certain limit, even a minor bump to the skull can cause them to snap and bleed into the subdural space between the inner skull surface and the brain.
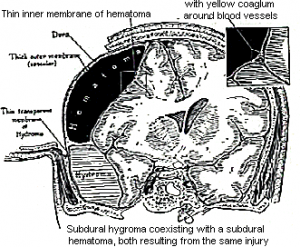
With the body's excellent blood-controlling mechanisms at work, the first few “episodes” may go unnoticed, since there is plenty of room for the blood.
However, with repeated episodes, a critical volume is reached, and the brain is compressed.
This is the time that the lady awakens with a noticeably malfunctioning brain–slurred speech and a wobbly gait.
More often than not, these chronic Subdural Hematomas are not fresh clots, but rather liquefied, old blood mixed with some fresh blood.
Thus, they can be easily drained by a very small hole in the skull.
In fact (see History), the earliest operations known to man were done for this reason. More than 3,000 years ago, many people including the Incas of South America and the Sumerians of the Middle East performed these operations called trephination, in the hopes of expelling evil spirits from the brains of men they felt were possessed.
Many such skulls have been found at archeological digs the world over. These operations were often successful even then.
OTHER CAUSES
- Major Trauma
By far the most common cause of a subdural hematoma is severe brain injury after a road traffic accident or a fall from a great height.
These traumatic subdural hematomas are always associated with considerable brain damage and occur immediately after the injury.
These injuries will be further addressed under the heading of Brain Injury (under construction).
- Spontaneous Acute SDH
Occasionally an artery on or near the surface of the brain will burst, causing a very large and emergent subdural hematoma to develop.
These are due to vascular malformations of the brain (e.g. aneurysm, AVM, dural AVM), containing a threat for future bleeding.
Because of the high pressure (and therefore volume) and rapid expansion of these SDH's, the patient is most often in serious trouble, requiring emergency surgery to be performed.