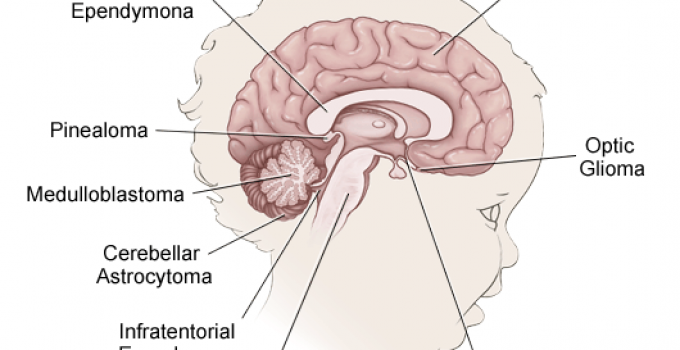
The image below reveals the most common locations for brain tumors in children. The peak incidence occurs in the early years of childhood and dips to a minimum in the teen years.
The most commonly found brain tumors in childhood include infratentorial (70-80%) such as Medulloblastoma and Glial tumors and are followed by Germ cell tumors and Craniopharyngioma.
Children have a greater chance of responding better to curative treatment than adults.
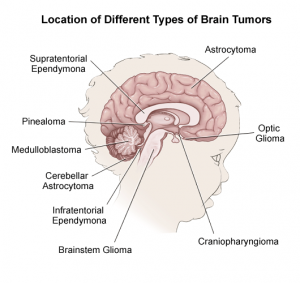
Table of Contents
Incidence Of Brain Tumors in Children
Benign and malignant tumors of the brain and CNS account for roughly a quarter of all cancer cases seen in children.
The rate of incidence witnessed in the United Kingdom is approximately 5 per 100,000 kids aged between 0-9 years.
Out of all CNS and brain tumor cases in young children, 43% consist of Astrocytomas, which are frequently ‘low grade’ tumors and rarely exhibit signs and symptoms of high (fast-growing) grade tumors.
Tumors of the Ependymoma and Choroid plexus are seen in children less than one year of age.
Etiology – (The Cause Of The Tumor)
The exact underlying reason for the initiation of brain tumors has not been found out. A definite correlation between certain inherited illnesses and brain tumors has been noticed.
For example- The frequency of incidence of Astrocytomas elevates young patients suffering from Neurofibromatosis. Similarly, those having Von Hippel-Lindau disease have greater chances of being afflicted by a tumor known as haemangioblastoma.
Genetic mutations in those genes that function as tumor suppressants such as retinoblastoma gene are suspected. The majority of brain tumors seem to be sporadic in origin.
A medical history of certain conditions such as the removal of adenoids or tonsils predisposes your child to solid tumors.
No definite conclusion has been reached and research continues. The incidence rate and frequency of some common childhood brain tumors are as follows-

Tumors located in the hemispheres: Gliomas
Tumors located in the midline: Chiasmal Gliomas, craniopharyngiomas and tumors in the pineal region.
Tumors developing in the posterior fossa: Brainstem Gliomas, Medulloblastoma, ependymomas, and cerebellar astrocytoma. (In descending order of incidence rate)
Clinical Features
The symptoms described below are commonly experienced by most patients, though they will vary with each child.
Other factors that determine the extent or intensity of symptoms experienced include the size of the tumor and its location as well as the increased pressure in the limited space.
The presence of extra fluid or tissue in the delicate structure of the brain and blockage of one or a few ventricles that normally drain out the fluid poses another problem. It pushes the intracranial pressure to beyond normal limits.
This pressure gives rise to episodes of headache which cause the most pain in the morning, vomiting, changes in personality and feelings of drowsiness.
The patient may experience depression too. Respiratory and heart functions get impacted.
Tumors in the front portion (cerebrum) of the brain cause the following symptoms: changes in vision, speech, seizures, confusion and a decline in strength or paralysis of one half of the entire body.
If the middle portion (brainstem) is where the tumor is situated, some of the features are:

Double vision, fits, intense headaches, changes in respiration plus endocrinal disturbances in the form of diabetes.
Cerebellum tumors cause a gradual loss of co-ordination over muscular movements, vomiting but without nausea (frequently in the morning time), ataxia (disturbance in the function of walking) and headache.
Impaired concentration, loss of weight, excessive sleeping are some of the other symptoms to note.
If your little one has recently been complaining of any of the above, make sure you consult a child physician for examination and diagnosis of the underlying cause.
Signs Of Brain Tumors in Children
Get a physical examination if you notice a few important changes in your child’s health.
For example, an outward curving of your infant’s fontanelle (a soft spot) that looks like a prominent bulge, larger than normal eyes, etc.
If the health care provider notices a lack of reflex in your child’s eye, Babinski’s reflex or sutures that are separated, he will ask for a few tests to be done such as CT scan and an MRI of the head.
If diagnosed with a brain tumor, go in for treatment as early treatment dramatically improves the chances of complete recovery.
Proper management includes treatment of cancer plus complications and moral support to the child.
Specific treatment of brain tumors is based on your child’s health status, previous and current medical history, the extent of damage caused to your child’s level of tolerance towards medical and surgical procedures, medications, etc and your personal opinion.
Surgical resection is the main mode of treatment, which involves the removal of the tumor mass.
There are certain cases for which surgery is not a possibility due to the risky location of the tumor, such as brainstem gliomas. Other modalities of treatment combined with surgery include chemotherapy and radiotherapy.
Removal of the abnormal collection of tumor cells while preserving neurological function is the ultimate goal of surgeons.
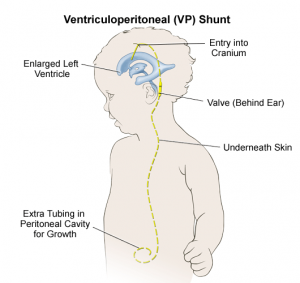
Partial removal is sometimes the only option. To control the mounting intracerebral pressure, neurosurgeons will install a shunt.
Chemotherapy
Many chemotherapy regimens are in use nowadays and involve Vincristine. In cases where partial excision has been carried out, the residual tumor cells are destroyed via chemotherapy. Drugs like Cyclophosphamide and 5- Fluorouracil is new and effective.
Radiotherapy
This treatment is provided in comparatively low doses to localized areas of the brain to prevent damage to normal tissues. In a few slow-growing brain tumors, interstitial seeds are incorporated in the site of operation during the operation.
Medications
These include corticosteroids such as Dexamethasone to relieve the pressure caused by brain swelling. Mannitol and urea act as effective diuretics to decrease both, the elevated pressure and swelling. Seizures need to be treated via anticonvulsants such as phenytoin etc.
The overall prognosis depends to a great degree on the type of tumor, its location and size. Other factors include the presence of metastasis and responsiveness of the brain tumor to surgery.
Prompt treatment and aggressive medical therapy is a must for a favorable prognosis. Periodic follow-up care must not be overlooked.
The Worst News For Any Parent To Hear
“I am truly sorry, but your child has a brain tumor…”
The world of childhood brain tumors has no “Welcome” sign leading into it.
No matter what anyone says to minimize the situation, this statement is the most painful sentence a human can hear. The combination of fear, shock, and pain can be too much to bear.
“To see such innocence, so roughly shaken by this terrible trial, at such a young age, is nothing short of incomprehensible.” I still hear this sentence, uttered by a visibly shaken parent.
Instead of becoming more routine and distant, the visceral terror that it engendered in me (the supposed all-knowing physician/advisor), my delivery of such information has grown more and more difficult, even personal. I watch my own small children grow and develop.
As a physician, one realizes that more than ever, there is no place for impersonal behavior when caring for the children who are afflicted by a brain tumor, benign or otherwise, and for their families as well.
No amount of experience or training can help one to ease or minimize the situation.
When we discuss special areas such as:
- Outcome: Do “excellent long-term results” mean a ten-year survival for a 3-year old– your child living long enough to be frustrated by death at the age of thirteen? We parents think only of 50 and 60-year plans. Five- and ten-year plans are unacceptable. We want to know that our grandchildren will not live to see their parents die at a young age.
- Quality of life: Does that mean that a 5-year old child will have no hair, be skinny and slow to walk and play with his friends and classmates? How can we parents bear to live through the process of trying to give our child a childhood instead of a world of I.V. tubes, doctors who speak of life-and-death, hospital corridors and toys that our children will never play with?
- Doctors: Who are they? Can we do anything to keep them human, warm, and caring for our child? How do we deal with our own resentment for the fearful news, difficult therapies, and their human frailty? How do we keep our child happy to see them? Most children cringe at the mere mention of visiting a doctor-with-a-shot-to-give, or a visit to the dentist with his drills and instruments.
- Hospitals: How do we keep these innocents away from such large and frightening monoliths?
- We parents: How can we possibly bear all of this without frightening our little, loving child?
- Hope: Yes, there IS hope! Your child is truly a precious gift. No matter what cards we are dealt with, a child's joy and innocence are somehow never lost. In the worst of times, a child's pain often becomes the parent's teacher. And when we expect the best for our children, we often get it despite all odds.
THE BIOLOGY OF CHILDHOOD BRAIN TUMORS
Pediatric brain tumors are different
Most frequently, they come from “young” cells. These are cells are still developing (“immature” or “primitive” cells) and have not reached full maturity. They are developing at the same time as the child is developing.
If one looks at the way a normal cell matures from its very beginning as a “primitive” brain cell (a precursor) through its stages of normal development, towards becoming an adult cell type, one can start to understand the logic of the progression of tumor types in children.
A diagrammatic representation of the manner in which brain cells develop from the embryo to the adult is under construction and it will be posted soon.
For every normal cell type, there is a corresponding tumor that can arise from it.
Thus, there is the primitive neuroectodermal tumor (PNET), the medulloblastoma, the astroblastoma, the neuroblastoma, the astrocytoma, the gangliocytoma/neurocytoma, the ependymoma, and so on.
There are also other unusual tumors such as the teratoma, the pineoblastoma, the esthesioneuroblastoma, etc.
There are also other tumors that come from non-brain origins such as pituitary tumors, teratomas, meningiomas, skull bone tumors, and blood vessel tumors such as hemangioblastoma or cavernous angioma.
Children commonly have brain tumors such as the PNET, medulloblastoma, various embryonic tumors and unusual tumors of the developing brainstem, hypothalamus and optic nerves (juvenile pilocytic astrocytomas, teratomas, etc.)
There are variations of these tumors and they are rare as well as difficult to understand.
Parents and children should ask as many questions as possible. The questions can help them reach a level of comfort, confident that the problem is clearly comprehended.
Knowledge of the expected and the potentially unexpected will allow you to guide your child through the process of the battle against their brain tumor.
No matter how harried, tired or busy your surgeon and doctors might seem, it is important to understand the problems fully.
This will make the efforts of all involved more effective. More often than not, knowledge helps us cope with the developing situation better.
The most important point is that some of these tumors hold the promise for a true and complete cure!
There is nothing more satisfactory than the complete removal of a dreadful sounding cerebellar microcystic astrocytoma or a hemangioblastoma.
Families soar from the depths of despair to the heights of sublime elation when the smiling surgeon comes to the waiting room after a difficult surgery. The surgeon may not look tired at all.
The smile-on-his-face says that he has just had the privilege of completely removing a tumor!
MEDULLOBLASTOMA
This tumor is probably the most common tumor of children. It arises from one of the “junior” cells of the developing brain, called the medulloblastoma.
This tumor almost always grows in the middle of the cerebellum (the balance part of the brain, in the back, behind the brainstem).
More often than not, small children are found to have the tumor only after it has caused secondary problems relating to blockage of the normal flow of cerebrospinal from the ventricles to the drainage system located along the outer surface of the brain (obstructive hydrocephalus).
This results in headaches, visual problems, and decreased alertness.
Often, parents will notice “sundowning”, (the eyes are “stuck” in the downward gaze position) of the baby's eyes, due to local pressure on one of the brain's centers for eye control.
EPENDYMOMA
The ependymoma arises from the cells that line the internal surfaces of the brain. These cells line the fluid spaces of the brain (ventricular system) and are relatively few in number.
Some of these cells are quite specialized, having little frond-like protruberances that move the cerebrospinal fluid as it permeates into the brain from the ventricular system and back again.
These tumors are rare.
They are usually found on the internal surfaces of the brain and spinal cord, such as the fourth ventricle of the brain (in the back, inside) and within the central canal of the spinal cord.
Occasionally they grow just beneath the surface of the lateral ventricles (called “subependymoma”).
Although these tumors are capable of malignant behavior, they are almost always benign. Surgical removal often leads to a cure, especially when the tumor arises right from the surface to the fluid spaces of the brain and grows into the ventricles, an “exophytic” growth, allowing for complete removal.
If you or your child has this tumor, be confident that the future holds promise.
CEREBELLAR ASTROCYTOMA
This tumor is quite curable. The small cyst version is one that, when surgically removed, is gone for good.
Forget about all the fears and just thank God that your child will do well. Even if the MRI or CAT scan shows a large cyst with surrounding tumor or a tumor “nodule” in the wall of the cyst, the surgery can go well.
When the tumor is the more aggressive type, the outcome depends on the grade/size of the tumor.
TREATMENT OF CHILDHOOD BRAIN TUMORS
The treatment of these tumors usually include a combination of approaches, each tailored to deal with the problems that children are presented with:
- Surgery: In some cases the definitive treatment is surgery. In most, however, surgery serves as a temporizing measure that will keep a child out of trouble for long enough to get through definitive therapy that will hopefully eliminate the tumor. Brain surgery is usually the easiest part of a child's treatment.
- Shunting: Quite often (e.g. medulloblastomas) childhood tumors present the blockage of the fluid spaces of the brain, (obstructive hydrocephalus). In shunting, a thin silastic tube (the shunt) is placed into the fluid spaces of the brain and passed under the skin into the child's abdomen where the fluid is absorbed.
- Chemotherapy: Unfortunately, chemotherapy is the hard part of brain tumor treatment. It is only required for more aggressive tumors. As a rule, chemotherapy should be even more aggressive than the tumor itself. The trials which are imposed both on the child and parents are many. Bravery and an unremitting attitude of hope are required by all involved.
- Radiation: Because the developing brain of a child is so very sensitive to radiation therapy, it is deliberately limited. The irony of effective radiation therapy is that when it works well, the brain damage it causes might exceed that done by the original tumor. More often than not, your doctor will recommend that if any radiation is to be given, it should be held off until the child has grown older and the brain has sufficiently matured.
The good news is that REAL HOPE exists. Long term results are becoming more and more common, some children surviving fifty years and beyond.
This has become especially true with wonderful improvements in chemotherapy and surgical techniques. The promise of cures for difficult tumors is becoming a reality for more families than ever before.
Resources:
- https://www.clicsargent.org.uk/types-of-cancer/brain-and-spine-tumours/
- https://www.thebraintumourcharity.org/brain-tumour-diagnosis-treatment/types-brain-tumour-children
- http://www.brainstrust.org.uk/little-brainstrust/index.php
- https://www.teenagecancertrust.org/get-help/ive-got-cancer/types-cancer/brain-tumours
- https://www.stjude.org/