A Glioblastoma Multiforme is categorized as a grade IV astrocytoma and is also called glioblastoma or GBM. There are numerous variants of malignant or cancerous brain tumors.
Usually, a brain tumor is named after the cell type it originates from.
The most commonly occurring brain tumors are called gliomas, named after the glial cells, which nourish and safeguard neurons.
An astrocytoma is a glioma that builds up from the star-shaped glial cells (astrocytes).
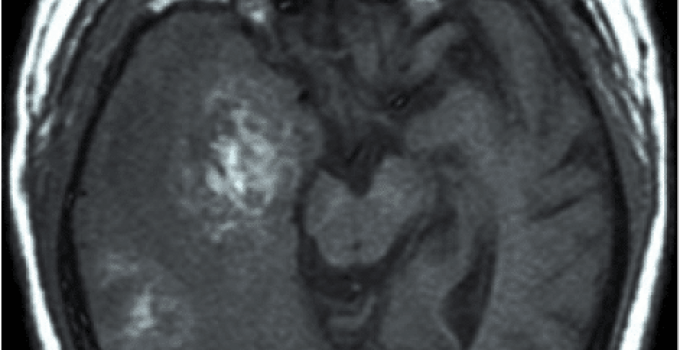
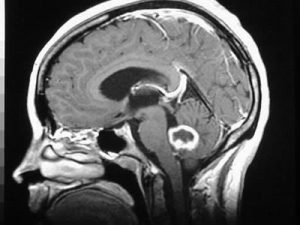
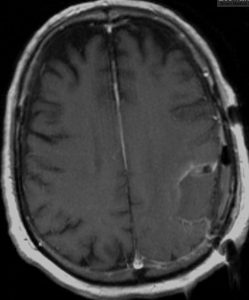
Coronal MRI with a contrast of a Glioblastoma WHO grade IV
Table of Contents
Glioblastoma Multiforme Characteristics
- Most invasive type of glial tumor
- Generally spreads to tissues nearby
- Huge potential for rapid growth
- Comprises discrete genetic subtypes
- Could be made up of quite a few dissimilar types of cells (i.e., astrocytes, oligodendrocytes)
- Might have developed from an astrocytoma or an oligodendroglioma at its initial stage
- Generally occurs among people in their fifties to seventies
- The average age of diagnosis is 64
- More frequent in men as compared to women
- Rare in children, constituting about 3% of pediatric brain tumors
- 17 % of major brain tumors are of this type
The Occurrence of GBM
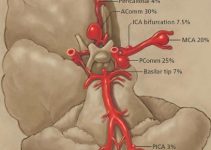
GBMs usually initiate in the cerebral hemispheres of the brain, however, they can also arise in the brainstem — the posterior part of the brain connecting with the spinal cord structurally, the cerebellum, which plays a significant role in motor control or the spinal cord.
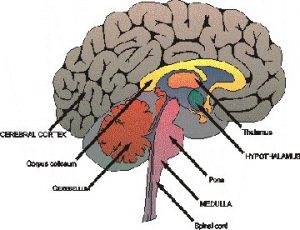
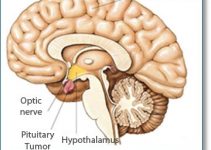
The Human Brain
The Human Brain with the Cerebellum in Purple
GBM Symptoms
GBMs may surface as frequent intense headaches due to the rise in intracranial (inside the skull) pressure, recurring memory loss, convulsions, personality disorder and difficulty in synchronization. GBM is hardly ever known to spread to different parts of the body.
The Causes Of GBM
Currently, the exact causes of the occurrence of a GBM are unknown. Extensive research has shown exposure to radiation, continuous contact with electromagnetic fields, extensive use of cell phones, hazardous chemicals and heredity as possible factors.
Identification Of GBM
A brain tumor is primarily identified with the aid of MRI (Magnetic Resonance Imaging) and a CT (Computerized Tomography) Scan. As well, a sample of the brain tissue is tested for the possibility of GBM.
The GBM has a distinct form, so it is easy for an oncologist to identify it in an MRI; however, a biopsy and a subsequent pathological report is a must for confirmation.
If the doctor feels that the tumor is operable, a biopsy is carried out at the same time as the surgery. For inaccessible tumors, a stereotactic or needle biopsy is used as an alternative.
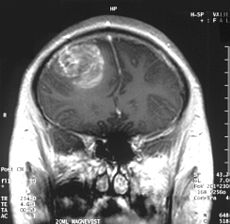
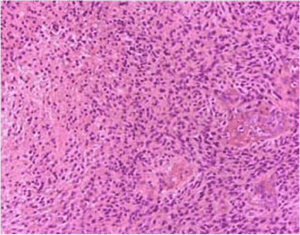
Glioblastoma Multiforme
The Recent Research
The latest research has revealed that there are various subtypes of GBM based on the intensity of their aggression. Studies are being undertaken to devise effective personalized treatment of GBM for each sub-type.
Treatment Of GBM
The treatment of a brain tumor depends on the form, extent, and position of the tumor. Typically, surgical treatment is carried out, and the patient is subsequently treated with radiation therapy or its combination with chemotherapy.
Removal of the tumor by surgery cannot cure the patient completely because, by the time a tumor is detected, the malignant cells may have rapidly spread to other parts of the brain and started to multiply.
If the doctor deems it appropriate, surgery may not be considered as an option. Instead, the administration of radiation therapy in conjunction with or followed by chemotherapy is carried out.
These methods are executed to destroy the cells that may have spread to other tissues in the brain.
Many clinical experiments using radiation, chemotherapy, or the right mix of both are carried out for preliminary and recurrent GBM.
Medical trials employing molecularly targeted remedies, successful in the treatment of other forms of cancer, are also being tried on GBM patients.
A standard procedure to treat GBM includes administration of radiation therapy five days a week for six weeks, along with oral chemotherapy with a drug named Temozolomide for five days a month.
The dosage and frequency of these therapies are at the discretion of the oncologist.
Along with this treatment, patients’ blood counts are periodically scrutinized and MRIs are executed periodically to observe the tumor’s reaction to treatment.
The process of treatment is aimed at curbing further spread of the tumor and alleviating symptoms with a minimum of side effects.
Glioblastoma Multiforme (GBM)
Malignant glioma, or glioblastoma multiforme, is the most aggressive form of the astrocytoma group of brain tumors and represents more than 66% of all cases of brain astrocytoma.
The survival rate of this tumor is extremely low because of its high-grade status and aggressiveness.
Epidemiology:
Glioblastoma is considered the most common primary brain tumor as it accounts for more than 12% of all brain tumors. In the USA and Europe, 2-3 new cases are diagnosed annually in every 100,000 people.
Race:
Glioblastoma multiforme is more common in whites.
Sex:
Malignant glioblastoma is more common in males when compared to females with a male to female ration of 3:2.
Age:
Glioblastoma multiforme can affect a person of any age; however, it is rather more common between 45 and 70 years. Less than 9% of all patients diagnosed with malignant glioblastoma are children.
Clinical Picture:
Patients start to complain less than 3 months before the diagnosis is established in about 50% of cases, except if the tumor is the result of a transformation of a low-grade astrocytoma which has been present for some time.
- A gradually progressing neurological deficit is the most common presenting complaint of patients with malignant glioblastoma. This is mostly in the form of muscular weakness. On the other hand, headache is the most common symptom experienced by most patients.
- Occasionally, patients present with manifestations of increased intracranial tension such as cognitive impairment, nausea, vomiting, and headache.
- Seizures are also common in some patients.
- Headaches are usually severe early in the morning or shortly after waking.
- Changes in mood, personality, mental abilities, and concentration can be observed early on, or maybe the only symptoms present.
- Occasionally, a patient complains of focal neurologic deficits that reflect the site of the tumor. Focal manifestations include weakness, paralysis, loss of vision, sensory loss or aphasia.
Imaging Studies:
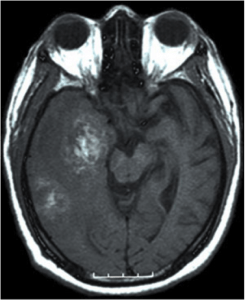
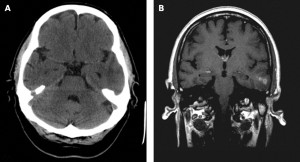
CT scanning can show the tumor and its extension; nevertheless, it can miss small tumors, so it is not an accurate tool in establishing the diagnosis of glioblastoma multiforme. It must be kept in mind that a missed low-grade glioma can progress to more aggressive forms of glioblastoma multiforme.
MRI is much more sensitive to the existence of the tumor. Furthermore, MRI can help visualize edema around the tumor, when present.
Accordingly, MRI is the imaging study of choice when a diagnosis of glioblastoma multiforme is suspected. Malignant glioma is a highly infiltrating tumor, so tumor cells are often present beyond the margins delineated by an MRI scan.
Metastasis (spread of the tumor outside its primary location) is frequent in other parts of the central nervous system (CNS).
Post-operatively, MRI is not accurate in differentiating scar tissue from recurrent tumors, while positron emission tomography (PET) is very helpful in this regard.
Malignant glioblastoma can assume different shapes, so it can be confused with other disorders such as an abscess, an infarction or lesions associated with multiple sclerosis, which can lead to delay in establishing a diagnosis.
The following generalizations are very helpful in differentiating glioblastoma multiforme from low-grade astrocytoma:
– The incidence of calcified lesions is higher in low astrocytoma when compared to glioblastoma multiforme.
– The incidence of increased enhancement (special appearance due to absorption of brain tissues of a dye used during MRI scanning) is higher in glioblastoma multiforme when compared to low-grade astrocytoma.
– The incidence of necrosis, hemorrhage, edema and mass effects follow the same pattern as that of enhancement.
A few forms of malignant glioblastoma can be considered variants. For instance, monocellular glioblastoma, or giant cell glioblastoma, is often considered a variant of malignant glioblastoma, although it has the same MRI findings of malignant glioblastoma.
Radiography:
X-rays are not often used in the workup of a patient with a malignant glioblastoma. Nevertheless, when the tumor is very aggressive, with an invasion of the skull bones, skull erosive changes can be demonstrated on a skull x-ray. Very rarely, the tumor sends metastasis to limb bones which can be also visualized on plain x-rays.
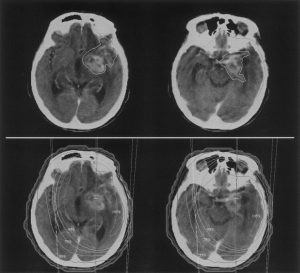
CT Scanning:
CT scans are often helpful in the diagnosis of malignant glioma. On the other hand, the CT appearance of some brain lesions may mimic that of malignant glioblastomas such as tumors other than malignant glioblastoma, infarction with hemorrhage and brain abscess. Glioblastoma multiforme can sometimes assume a multi-focal distribution which can be indistinguishable on CT images from diffuse forms of multiple sclerosis.
The findings of malignant glioblastoma on a non-enhanced CT scan include the following:
– A mass with poorly defined margins.
– A lesion with areas of fluid attenuation which is present in about 95% of cases.
– A calcified lesion which is rather rare except if the tumor is the result of the transformation of another tumor such as low-grade astrocytoma.
– Marked mass effects and edema.
Enhanced CT scans findings include inhomogeneity and irregularity, solid enhancement, ring enhancement, and little enhancement when the tumor assumes a diffuse form.
Magnetic Resonance Imaging:
MRI is the best imaging modality in the diagnosis of malignant glioblastoma; however, brain lesions with hemorrhagic parts can resemble malignant glioblastoma on MRI.
On MRI, glioblastoma multiforme shows heterogeneous masses with areas of cystic changes, edema in the tissues surrounding the tumor, areas of necrosis, new vessel formation and pressure effects on the nearby brain structures.
Nuclear Imaging:
Positron emission tomography (PET) imaging is a useful imaging modality in the evaluation of glioblastoma multiforme, especially after surgical resection. In such situations, the differentiation of non-excised tumor residual or recurrent tumor from scarring or postoperative edema is possible. Malignant glioblastoma is viewed during PET scanning because of the high metabolic rate and glucose consumption of the tumor cells.
Whenever a recurrent tumor is suspected, increased tracer tissue uptake at the site of previous surgical resection is often diagnostic. Nevertheless, following radiotherapy increased uptake at the surgical site can occur regardless of tumor recurrence. Epiliptogenic activity near the site of surgery can exhibit increased tracer uptake, especially when high epileptic activity is noted.
Treatment For Malignant Glioblastoma
Treating malignant glioblastoma is not easy, especially since there is no curative treatment for it at the present time.
After establishing the diagnosis of glioblastoma multiforme, the treatment plan should include:
– Maximal surgical resection.
– Radiotherapy.
– Adjuvant and concomitant chemotherapy with temozolomide.
If the patient is older than 70 years, less aggressive lines of treatment are recommended such as temozolomide or radiation therapy.
Facts about Surgery On Glioblastoma Multiforme
There are various factors that determine whether a tumor is operable or not. The position of the tumor, its propinquity to critical organs, the extent of its spread and its connection to blood supply within the brain are the major determining factors.
Advanced technologies employed in operating procedures enable neurosurgeons to perform surgery on the smallest patch of tissue with the greatest precision. Sophisticated surgical microscopes, interactive MRIs and brain mapping techniques are employed to perform surgery with maximum accuracy.
Though the idea of brain surgery is quite frightening, talking out one’s anxiety and discussing doubts openly with the doctor can provide relief, and contacting other brain tumor survivors can also be of great help.
GBM Post Successful Surgery
Facts about Radiation Therapy
A suitable course of radiation therapy is planned by a radiation oncologist and a neurosurgeon. The aim is to destroy the cancerous cells without damaging the normal brain cells.
The current radiation therapy technologies being used are 2D coplanar treatment, 3D conformal treatment, intensity-modulated therapy, and stereotactic radiosurgery.
Radiation Therapy
Facts about Chemotherapy
Under Chemotherapy, a neuro-oncologist prescribes drugs orally or as venous injections to destroy the maximum number of remaining tumor cells. Chemotherapy can also be directed at the tumor site during surgery in the form of biodegradable polymer wafers.
GBM after treatment
Research is now investigating the possibility of using focal radiation, which is directly delivered to the site of the tumor using an implanted balloon that contains the radioactive substance.
Bevacizumab is an anti-angiogenic agent that has been recently approved by the US Food and Drug Administration for the treatment of recurrent glioblastoma multiforme.
There are other lines of treatment that are still under research, including dendritic cell and peptide vaccines, gene therapy, radiolabelled drugs, synthetic chlorotoxin, and radiolabelled antibodies.
Possible Side-Effects
Though chemotherapy and radiation therapy are aimed at destroying malignant cells, they can end up wiping out healthy cells as well.
These treatments may cause increased fatigue, hair loss, and dryness of scalp, nausea and a certain extent of immunity loss.
Currently, many drugs are available on the market to assuage the possible side-effects of the heavy drugs used in the treatment of GBM.
A patient can conduct an open discussion about treatment and drug administration, its possible side-effects, potential benefits and future course of life with the treatment team.
This will provide the patient with insights regarding treatments that will relieve anxiety and stress.
References:
- https://academic.oup.com/nop/article/3/1/29/2460149
- https://moffitt.org/cancers/glioblastoma/treatment/chemotherapy/
- https://www.cancercare.org/support_groups/tagged/glioblastoma
- https://braintumor.org/brain-tumor-information/finding-support-coping/
- https://rarediseases.org/rare-diseases/glioblastoma-multiforme/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5681990/