Ependymoma brain tumors arise from a special type of cell in the central nervous system (CNS) known as the ependymal cells. Ependymomas were first discovered by Bailey in the year 1924.
Ependymoma brain tumors can arise in the brain (intracranial) or the spinal cord. Ependymoma can affect children, which is intracranial in about 90% of cases. Nonetheless, in adults, 75% of all ependymomas arise from the spinal cord.

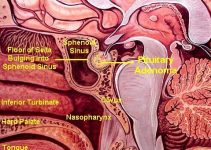
Gross anatomy of ependymoma of the 4th ventricle
Pathophysiology:
Ependymoma brain tumors are believed to grow in response to special genetic conformations that change normal ependymal cells into tumor producing cells. The precipitating factors and the precise scenario of those genetic changes are not completely understood; nevertheless, some studies have delineated the mutations incriminated to promote the growth of various tumors.
Chromosomal translocations (i.e. replacement of normal parts of a chromosome by other forms of genetic material) that involve chromosomes 22, 17 and 9 are common among patients with ependymomas. Moreover, loss of parts of chromosome 17 has been also reported in ependymoma patients. Recently, loss of parts of chromosome 22 has been also associated with ependymoma.
Many genetic studies are still in progress to identify the relationship between tumor progression and specific genetic mutations. Presently, efforts are directed towards the discovery of genes suppressing the growth of ependymoma on chromosome 22.
Epidemiology:
Intracranial ependymomas comprise approximately 6% to 9% of all primary CNS tumors. In children younger than 3 years, ependymomas represent 30% of primary CNS tumors. The incidence is equal in females and males.
Mortality and Morbidity:
The 10 year survival rate of ependymoma ranges from 45% to 55%. When survival rates of children and adults are combined, the 5 year survival rate of ependymoma is about 50%.
Age:
Ependymoma affects children who are usually diagnosed at the age of 4 years; however, in 25% to 40% of cases, patients are below 2 years of age. Spinal ependymoma usually affects patients between 15 and 40 years.
Clinical Picture:
The symptoms and clinical signs of ependymoma vary according to the site of the tumor and the age of the patient on presentation. Prior to diagnosis, the symptoms will usually have been present for a duration ranging from 1 to 36 months.
– In children, the tumor occasionally arises from the 4th ventricle (a fluid filled cavity within the brain) which causes an increase in intracranial pressure leading to headache, lethargy, nausea and/or vomiting. If the tumor grows further, affection of the cranial nerves VIII (responsible for conveying hearing sensation and body balance (proprioception)) and X (contains the body’s main autonomic parasympathetic nerve fibers).
– If the tumor starts growing in a child before closure of the of the skull sutures, progressive enlargement of the head circumference may be manifest.
– Supratentorial ependymomas (located in the upper parts of the brain) can also increase the intracranial pressure which is usually manifested as nausea, vomiting, headache and cognitive impairment (memory, decision making, calculation skills…etc). Moreover, supratentorial ependymomas can lead to loss of vision, sensory loss and aphasia (impaired speech).
– Spinal ependymomas are usually associated with weakness, sensory loss and/or parasthesia (abnormal sensations) that are located in an area corresponding to the level of the spinal cord affected by the tumor.
Imaging Studies:
CT and MRI are very helpful in the diagnosis of ependymoma. If ependymoma is suspected, MRI should be done without using an intravenous contrast (dye used to enhance the brain tissues during MRI scanning).

CT scan showing 4th ventricular ependymoma
Treatment:
Medical treatment:
The medical treatment of patients diagnosed with ependymoma includes:
– Steroids to manage edema of the brain tissue near the tumor.
– Anticonvulsants for patients complaining from convulsions.
– Adjuvant therapy which includes chemotherapy, radiosurgery and conventional radiation treatment.
Many neurosurgeons don’t approve of adjuvant therapy for ependymomas confirmed by histological examination (microscopic examination of a tumor specimen).
The National Comprehensive Cancer Network (NCCN) recommends the following for adult patients with ependymomas:
– Grade II WHO ependymoma: gross total surgical resection can be followed by limited field fractionated external beam radiotherapy (LFFEBRT). However, if MRI scanning shows subtotal excision of the tumor, LFFEBRT is mandatory.
– Grade III WHO anaplastic epndymoma: LFFEBRT should follow gross surgical resection whether or not the tumor had been completely removed on postoperative MRI.
– Recurrent ependymoma: Radiation therapy should be prescribed for patients who never received radiation therapy. However, if patients have received radiation therapy, supportive care or chemotherapy should be the other options.
Radiation therapy should be avoided in children below 3 years, because it can markedly affect the development of a growing brain. In those patients, a combination of chemotherapeutic agents is an effective alternative. 2 regimens are usually administered to children with ependymomas:
1- Etoposide, carboplatin, cisplatin, mechlorethamine and vincristine.
2- – Ifosfamide, etoposide and carboplatin.
In the year 2000, a group of researchers investigated the effectiveness of stereotactic radiosurgery (SRS) for patients with recurrent ependymomas and concluded that this therapeutic technique can promote salvage in some patients.
Adjuvant therapy is unhelpful for patients with spinal ependymomas after undergoing total surgical resection. If a tumor hasn’t been completely removed, or recurs after some time, radiation therapy can be used after careful evaluation of the patient’s neurological status and medical condition.
Surgical management:
The extent of brain tissues excised around an ependymoma can markedly affect the survival of patients after surgery; accordingly, gross total resection (GTR) is an ideal option. The surgeon should weigh the need for extending surgical resection against the possibility of injurying vital brain centers and cranial nerves.
Consultations:
A well organized team of specialists including a neurosurgeon, a neurologist, an oncologist and a radiation oncologist should carefully evaluate patients diagnosed with ependymoma, in order to create a successful treatment plan.
Following surgery, specialists of rehabilitative medicine and physical therapy should also be consulted to facilitate recovery.
Activities:
There are no universal activity restrictions indicated for patients with ependymomas.
– A patient’s activity level should be correlated with his/her neurological status and overall medical condition.
– If convulsions are present, operation of motor vehicles should be precluded.
Medications:
There are no specific pharmaceutical agents for the treatment of ependymoma; nevertheless, patients with supratentorial ependymomas usually need medical treatment. When seizures are present, patients are usually prescribed phenytoin (Dilantin), levetiracetam (Keppra) or carbamazepine (Tegretol). Levetiracetam is usually preferred over phenytoin and carbmazepine because they interfere with the actions of some anti-tumor treatment lines. Edema of the brain tissues secondary to the tumor can be treated effectively with corticosteroid agents such as dexamethasone.
Follow up:
Further inpatient care:
After surgical resection of an ependymoma, patients typically spend the first 24 hours after surgery in an intensive care unit followed by 3-5 days of hospital stay in the ward. The length of a patient’s stay is related to his/her medical condition, overall medical status, location of the tumor and extent of surgical resection.
Following surgery, antibiotics are administered for 24 hours. When the general condition improves, physical rehabilitation and occupational therapy should be started as soon as possible.
During the hospital stay, the patient should undergo a postoperative MRI to determine whether or not the tumor had been completely removed. Moreover, MRI of the spines should be done post-operatively to rule out the presence of tumor seedlings.
If not done before surgery, consultation of a neurologist, radiation oncologist and neurooncologist should be done.
Further outpatient care:
A rehabilitation team should follow up patients who still exhibit neurological deficits after surgical resection of spinal ependymomas.
Children should be carefully monitored for manifestations of increased intracranial tension. When anticonvulsant drugs are used, their blood levels should be checked regularly.
Complications:
Generally speaking, surgical resection of a brain tumor has a mortality rate of approximately 1% to 2%. About 40% of patients are healthy or exhibit minimal deficits following surgery. About 30% of patients have the same deficits manifested before surgery. 25% of patients manifest increased neurological deficits following surgery.
Bleeding, infection and deterioration of neurological deficits are the most common complications of surgical resection of brain tumors.
Resources: