The trigeminal nerve is the fifth in order among the cranial nerves and constitutes a mix of sensory and motor neurons. Any sensation that we experience in our face, as well as control of motor tasks like biting, chewing, and ingesting, are due to the trigeminal nerve or the fifth nerve.
Trigeminal neuralgia which is also called the suicide disease is a neuropathic condition. This disease is prone to frequent misdiagnosis and the actual number of cases may be quite higher than reported.
- It is distinguished by instances of extreme pain in the patient’s face, initiating at the trigeminal nerve.
- This is a rare disorder that is known to occur in only 1 out of 15,000 people.
- It is considered to be one of the most excruciating conditions occurring in human beings.
- It is usually known to occur past the age of fifty; however, it has been reported to occur at an age — as young as three years.
- It has been generally known to occur more in women than men.
The trigeminal nerve branches out majorly into the upper branch, the ophthalmic nerve — which is the middle one –- the maxillary nerve, and the lower branch, which is the mandibular nerve.
In Trigeminal Neuralgia, any one, two or all of these branches could be impacted, and 10-12% of reported cases are known to be bilateral, occurring on both the sides of a patient’s face.
Trigeminal neuralgia (TN) is usually known to involve the middle maxillary nerve and lower mandibular nerve.
The patient experiences intense pain in any or every part of the face.
TN or tic douloureux cannot be easily controlled and can only be handled with diverse treatment alternatives.
Table of Contents
Surgical Therapy
Experienced doctors recommend surgical treatment for Trigeminal Neuralgia only in case of an ineffective medical treatment. Along with pain relief, a patient might experience recurrent numbness post-surgery.
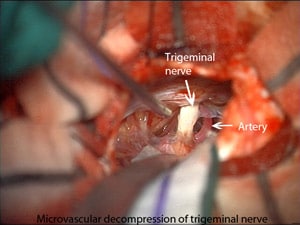
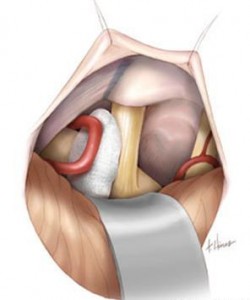
Microsurgical decompression of the Trigeminal Neuralgia produces relief from pain for the longest known duration.

Supralateral Cerebellar Approach
Other effective forms of surgery are percutaneous radiofrequency thermal rhizotomy and gamma knife technique; however, their effects are known to diminish with the passage of time.
According to a research report, out of 50 patients operated on with a Microsurgical decompression,
- 42 showed excellent results
- 5 showed good signs of recovery
- 2 suffered from the same condition after surgery
- 1 patient was cured following a second surgery

Of these patients, there were 29 females and 21 males in an age group of 31-73 years; 22 had pain in the right-side and 23 experienced it in the left-side of their face and the rest 5 had pain bilaterally.
The lateral decubitus position was preferred in these patients for reasons of safety in older patients and in others to avoid headaches after the operation.
Some surgeons also prefer having the patient in a sitting position during the operation.
Preoperative Administration and Surgical Technique
A pre-operative routine includes a Computerized Axial Tomography (CAT) scan and a series of diagnostic images of the skull.
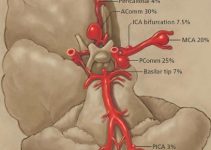
Angiography may also be needed in some cases to discount the incidence of any vascular anomaly. If a patient’s CT scan reveals the presence of an aneurysm, an angiography becomes essential for a detailed case analysis.
Drugs usually administered are:
- prior to and during the surgery – dexamethasone
- intra-surgical administration – 100 gm mannitol
- mechanical hyperventilation (Pco2, 25 to 30 mm of Hydrargyrum)
The operation is performed in the form of a suboccipital craniectomy, roughly 3 cm in diameter.
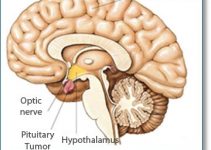
A straight paramedian incision is carried out, with the patient in a semi-prone position. Some patients may show the presence of other tumors that can be removed, resulting in a return to normal health. In other cases, the symptoms persist in spite of the removal of tumors that have no relation to the Trigeminal Neuralgia.
Operative Findings for Trigeminal Neuralgia
Research shows a majority of operative findings that consist of the branches of the superior or anterior inferior cerebellar arteries or veins compressing the point of origin of the Trigeminal Nerve.
Some patients might show an incidence of two blood vessels, both a vein and an artery, or both arteries, associated abnormally with the Trigeminal Nerve.
Results in Trigeminal Neuralgia due to Microsurgical Decompression
A majority of patients — around 84% — are known to completely recover with no pain in the facial region, no ensuing numbness and no further drug administration needed.
- 10% of individuals are known to encounter the minor sensations of pain in the facial region on rare occasions and may need either no or intermittent drug prescription.
- 2% of patients may need to undergo a second operation if the obstructing blood vessel is not recognized and decompressed at the first attempt.
- 4% of patients are known to demonstrate total curative failure with recurrence of severe pain.
A follow-up is essential for these patients, and the time for this usually ranges from a few months to up to five years.
Ensuing complications might consist of temporary CSF rhinorrhea, which is a serious condition causing the CSF – cerebrospinal fluid — to fill in the nasal cavity.
Another serious condition can be aseptic meningitis, in 4% of patients.
These 2 occurrences highlight the need for careful handling of the mastoid air cells and stopping the blood from entering into the subarachnoid region.
Limited hearing in 2% of the patients was also observed.
Fatalities are not known to occur during or after a microsurgical decompression.
This surgical procedure is safe and harmless and is not known to result in dysaesthesia. With the complete disappearance of pain in 84% of the cases, the rate of the reappearance of the pain at a later time is also known to be extremely low.
Conclusion
The gradual commencement of trigeminal neuralgia in an individual’s middle or later part of life and the turnaround of functional failure by the process of microsurgical decompression are known to be consistent with the vascular roots of origin for this disease.
However, the pathophysiological methods remain vague and doubtful. Cranial nerves have shown aberrations in their myelination in certain cases of trigeminal neuralgia.
However, its association with compressions in the circulatory system and the pathophysiological consequence is unclear.
References: